TREATMENT OF THYROID NODULE
Thyroid Nodules
Thyroid nodules are a common condition affecting the thyroid glands, with an incidence ranging from 20% to 76%. These nodules are observed in 50% of women and 30% of men, as detected through ultrasonography examinations.

While the majority (85-93%) of thyroid nodules are benign, they can still pose risks such as pressure symptoms, cosmetic concerns, and the potential to transform into malignant nodules. The risk of malignant transformation in thyroid nodules is approximately 5-15%.
Traditionally, treatment options for thyroid nodules include surgery and medication. However, surgery has its drawbacks, including the need for general anesthesia, potential hypothyroidism due to impaired thyroid function post-surgery, and scarring resulting from the procedure.
Ablation Therapy
Ablation therapy offers an alternative approach with several advantages:
- Fewer side effects and complications**
- Shorter hospital stays**
- No need for general anesthesia**
- Minimal scarring and maintenance of regular thyroid function**
Radiofrequency ablation (RFA) and laser ablation are the primary treatments for benign thyroid nodules. Additionally, microwave ablation serves as a secondary treatment method. The effectiveness of ablation in reducing nodule volume varies based on nodule size. For instance:
- In 10-12 ml nodules, the volume reduction rate ranges from 78% to 82%.
- In 20-30 ml nodules**, this rate is approximately 62-65%.
Patient Selection Criteria
Criteria for ablation include:
- Benign nodules confirmed by at least two fine needle aspiration biopsies.
- Presence of pressure symptoms or cosmetic concerns.
- Situations where surgery is not suitable or the patient prefers a non-surgical approach.
- Small, functioning thyroid nodules in young patients.
- Recurrent thyroid cancer cases with higher surgical risks, where ablation can be considered.
Which Cases Ablation is not Appropriate ?
Ablation is not recommended in the following cases:
- Very Large-Sized Nodules Extending into the Rib Cage: When nodules are exceptionally large and extend into the rib cage, ablation may not be appropriate.
- Suspicious Nodule Findings from Fine Needle Aspiration Biopsy: If fine needle aspiration biopsy results indicate suspicious nodules, ablation should be reconsidered.
- Recent Signs of Increased Thyroid Function (Hyperthyroidism): Patients with hyperthyroidism should avoid ablation.
- Previous Radiation to Head and Neck Segments: If a patient has received radiation therapy to the head and neck in the past, ablation may not be suitable.
- Life Expectancy Less Than 1 Year: Ablation should not be applied if the patient’s life expectancy is less than one year.
Patient Praparation and Thyroid Ablation Procedure
Before the procedure:
- Fine Needle Aspiration Biopsy: At least two fine needle aspiration biopsies should be performed before thyroid ablation, and cytology results should fall within the Bethesta 1-2 category.
- Laboratory Tests: T3, T4 levels, PT, PTT, INR, and hemogram blood tests are necessary.
Procedue Technique and Implementation
The ablation procedure does not require general anesthesia. It is performed under local anesthesia and sedoanalgesia.
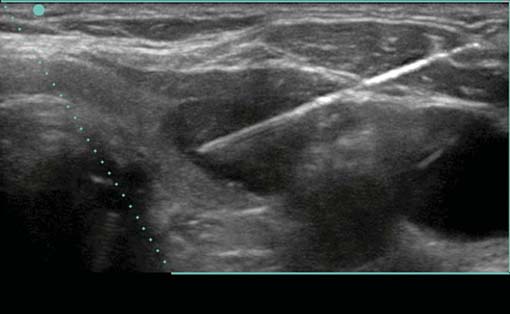
- Guided by Ultrasonography: The procedure is carried out daily, guided by ultrasonography.
- Post-Procedure Care: After ablation, applying an ice pack to the entrance area can prevent heat-related skin burns and bleeding.

Procedure-Originated Side Effects
Side effects are relatively rare:
- Mild Symptoms: Approximately 2 to 11 out of every 100 patients may experience mild symptoms such as pain or temporary thyroid dysfunction.
- Major Side Effects: In 0.5 to 1.6% of cases (5 to 16 out of every 1000 patients), major side effects may occur. These can include bleeding, hoarseness, eyelid drooping, and skin burns.
Monitoring
During the early period, ultrasonography checkups are performed in the third month after the procedure.


